
- Call : + 07523 300822
- Email : team@herefordshireurology.co.uk

Flow problems
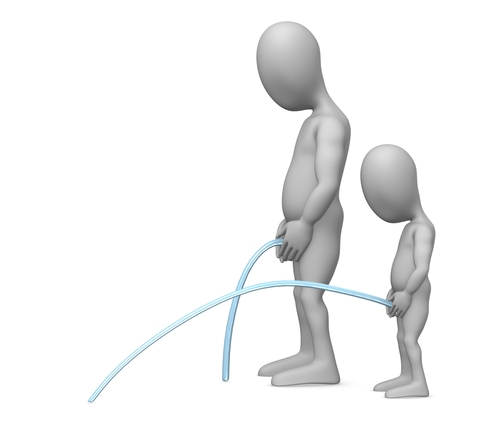
Problems with urinary flow are common and may affect both men and women. It is especially common in men as they age, in whom an enlarged prostate is the main cause of this problem. Other symptoms associated with a reduced urinary stream may include hesitation before starting to void, dribbling after finishing the void, incomplete emptying, and splitting/spraying of the urinary stream. Causes include prostatic enlargement or less commonly prostate cancer, narrowing (stricture) of the water pipe (urethra) in both males and females and other blockages such as stones or a tight foreskin in men.
If you are worried about your urinary flow, the best approach is to discuss this with your doctor.
Treatment
Poor urinary flow doesn’t necessarily require treatment, especially if it is not bothersome. However, they are some potentially serious causes and it is worth discussing this problem with a doctor. A medical assessment may include a discussion and examination by a doctor. Often urine and blood tests are requested, a questionnaire that scores the symptoms may need to be completed( IPSS Form ). To complete the investigations a flow test and a bladder scan are required to check what the flow is objectively like and the efficiency of bladder emptying. Very occasionally a cystoscopy is required to look at the water pipe and the bladder.
Once serious causes have been excluded, treatment depends upon the cause and may include observation, medication or surgery.
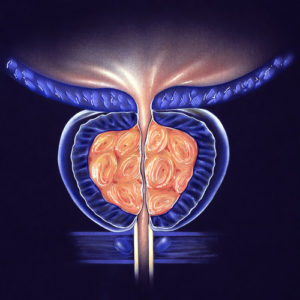
Prostate Cancer
Prostate cancer is the most commonly diagnosed male cancer in the United Kingdom. Approximately 37,000 men are diagnosed per year and 250,000 are living with the disease.
The majority of cancers are very slow growing and usually give no problems to start with, indeed some early cancers never cause problems and do not require treatment. The only sign of early prostate cancer may be a raised PSA blood test (prostate specific antigen). However some prostate cancers are aggressive and these are the ones that need to be identified and treated appropriately. When prostate cancers are advanced, they may cause urinary problems and may spread out of the prostate often to the bony skeleton.
Treatment depends upon the grade (aggressiveness) and stage (extent) of the cancer and there are a number of tests which may be required to diagnose and stage the cancer before discussing treatment.
Further useful information about prostate cancer is available on the MacMillan website and BAUS website. If you are worried about the possibility of having prostate cancer the best approach is to discuss this with your doctor.
Treatment
Treatment can be recommended to try to cure early prostate cancer that is contained within the prostate to stop it progressing, or to control cancer that has already spread outside the prostate.
There are a number of treatments that can cure early cancer the commonest include surgery or different forms of radiotherapy (which are often combined with hormone treatment injections). All these treatments have potential damaging effects and therefore, especially in early cancer that is at a low risk of causing problems, it may be suggested that it is better to not treat the cancer but to simply monitor it. This approach is called either active surveillance or watchful waiting.
More advanced cancer, which may have spread away from the prostate, and cannot be cured, is still treatable. Treatments may include hormone treatment, radiotherapy, surgery to improve urinary flow, or chemotherapy.
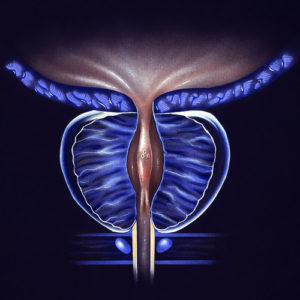
Prostate Enlargement
Approximately 50% of men will have an enlarged prostate by the age of 65. This is known as Benign Prostatic Enlargement (BPE). The enlargement may cause a number of difficulties but does not always necessarily lead to problems. Difficulties can include a slow urinary stream, hesitation before starting to urinate or dribbling after finishing, incomplete bladder emptying, a sense of urgency when needing to pass urine or passing urine frequently and having to get up at night to pass urine. Less common difficulties might include blood in the urine or semen, both of which need reporting to your doctor as they can be caused by other, more serious conditions.
If you are worried that you might be suffering from benign prostatic enlargement, it is worth discussing your problems with your doctor.
Treatment of an enlarged prostate depends on the severity of urinary difficulties that it causes. A medical assessment will be required to diagnose the problem and establish how severe the problems are. Enlargement can be managed in a number of ways, the simplest of which are simple lifestyle measures. For example paying attention to when and how much fluid is drunk. Most men that require treatment in addition to this respond to tablets. However in more severe cases (and especially if it is not possible to pass urine at all: retention) surgery may be required. Surgery is usually performed endoscopically –through the water pipe in the penis) and involves removing the central part of the prostate. This can be done using electricity and is known as a TURP (trans-urethral resection of prostate). A new surgical alternative is urolift which may have less side effects than conventional TURP will be coming soon.
Surgery is usually very effective at improving urinary difficulties caused by prostatic enlargement but does have more side effects than medication, the choice between treatment is best discussed on an individual basis with your urology consultant.
Prostatitis
Prostatitis means inflammation of the prostate gland which is situated within the pelvis just under the bladder. Prostatitis can be acute or chronic (lasting months or years). It is very common and can cause a number of symptoms which can include:
Acute prostatitis is often caused by infection, whereas chronic prostatitis (which is also known as chronic pelvic pain syndrome CPPS) is more likely to be caused by unresolved inflammation. If you are worried that you may have prostatitis it may be worth discussing the problem with a doctor.
Investigation of prostatitis starts with a discussion of problems and a medical examination. A questionnaire is often useful to establish the severity of the problems. Blood, urine and semen samples may be requested and an ultrasound scan may be requested. If the symptoms fail to settle with treatment further scans may be suggested as well as a telescopic examination of the water pipe and bladder (cystoscopy).
Acute prostatitis is often treated with appropriate antibiotics, painkillers and lifestyle advice. If the problem becomes chronic treatment becomes more difficult but various other treatments are available.
Raised PSA

PSA or Prostate Specific Antigen is a blood test used to look for prostate problems. Only the prostate makes this chemical in any quantity and some of it can be detected in the blood stream. The reason that PSA is of interest is that a raised PSA may indicate a prostate cancer, however, some people may have a normal PSA and have prostate cancer, conversely some patients will have an elevated PSA and not have prostate cancer. An elevated PSA suggests that there may be a prostate problem; this may simply be an enlarged prostate, an inflamed or infected prostate or prostate cancer. Hence PSA is prostate specific and not prostate cancer specific. It is worth bearing in mind that the higher the level of the PSA blood test, the more likely that cancer will be diagnosed.
As the PSA blood test may be elevated in a number of different prostate conditions, it is useful but may be difficult to interpret, and therefore may lead to a number of further tests designed to confirm or exclude the presence of prostate cancer. Ideally, only men that would benefit from being treated for prostate cancer should have a PSA test and this should be discussed with a doctor before a test. If you are unsure the prostate cancer risk management programme leaflet may be helpful.
A raised PSA blood test may need further tests to prove or exclude the presence of prostate cancer. A urine test may be performed to exclude active infection and a repeat PSA test is often requested to ensure that the first was a true reading. If the PSA is raised without an obvious source of infection or inflammation an MRI scan (Magnetic resonance Imaging) may be requested to look for any obvious abnormalities within the prostate with a view to performing Trans rectal ultrasound scan (TRUS) and prostatic biopsies to get some tissue for diagnosis.
The TRUS and biopsy test is designed to estimate the size and detect cancer of the prostate. However even this is not totally accurate and whilst a negative set of biopsies is reassuring it does not completely exclude prostate cancer.